Gum Disease Treatment Southern Pines, NC
Gum disease, or periodontitis, is a bacterial infection that affects the gum tissue and bones that support your teeth. Gum disease can have severe effects if left untreated. The infection can destroy the roots of your teeth, jawbone, and the surrounding soft tissue, leading to tooth loss.

Causes of Gum Disease
Plaque and Tartar build-up are the leading causes of gum diseases. Plaque is a sticky substance that forms on your teeth when food particles, oral bacteria, and saliva mix. Although regular flossing and brushing can prevent plaque build-up, it can still accumulate in hard-to-reach mouth areas, such as the back molars.
Tartar forms when plaque hardens after mixing with minerals from saliva in a process called mineralization. Tartar can create a conducive environment for oral bacteria by trapping food particles on the teeth’s surface. What’s more concerning is that tartar cannot be removed through brushing and flossing.
Tartar build-up can cause irritation, inflammation, and bleeding of the gums, which, if left untreated, can progress into advanced gum disease.
The onset of gum disease can be linked to several factors, including:
- Poor oral hygiene
- Smoking and tobacco use
- Hormonal changes
- Genetics
Types of Gum Disease
Gingivitis is a mild form of gum disease that occurs when plaque and bacteria accumulate on the teeth. It’s identified by symptoms such as swollen, inflamed, and bleeding gums. Fortunately, the effects of gingivitis can be reversed by maintaining good oral hygiene and scheduling regular dental check-ups.
While gingivitis doesn’t damage the bone structure and soft tissues supporting the teeth, it can progress into advanced gum disease (periodontitis) if left untreated.
Periodontitis is an advanced form of gum disease that results from the build-up of tartar under the gum tissue.. Over time, this can irritate the gums, causing them to pull away and create pockets along the gum line. Food particles and oral bacteria accumulate in these gum pockets leading to infection.
The immune system produces antibodies to fight the infection as the disease progresses. Unfortunately, the antibodies and toxins produced by the oral bacteria break down the gum tissue and bones supporting the teeth leading to weakened teeth and tooth loss.

Signs and Symptoms of Gum Disease
The common symptoms of gum disease include:
- Bright red, swollen, and puffy gums
- Bleeding gums, especially after brushing
- Persistent bad breath
- Pain when chewing
- Changes in teeth alignment
- Loose teeth
- Pus between your teeth and gums
Diagnosis of Gum Disease
To diagnose gum disease, your dentist will thoroughly evaluate your gums, teeth, and other oral structures. The diagnosis process generally involves the following steps:
Medical Background Check and Symptom Review
The dentist will begin by reviewing your medical history and identifying factors such as diabetes and medication that may make you vulnerable to gum disease. They will then check for gum disease symptoms such as swollen and bleeding gums.
Physical Examination
The dentist will physically examine your teeth and gums to determine their condition. They may use a dental explorer, a thin pointed tool to probe the affected teeth and surrounding gums. They will investigate further if they notice roughness on the teeth and gums or if you experience intense tooth sensitivity, as these signs could point to gum disease.
The dentist may also use a dental probe to evaluate the health of your gums. This involves checking for signs of bleeding, inflammation, and pus between the teeth and gums, as well as measuring the depth of gum pockets around the affected teeth.
The dentist will take dental X-rays to determine the extent of damage to the gum tissue and surrounding teeth.
Treatment Options for Gum Disease
Non-surgical Gum Disease Treatment Options
Professional Cleaning
If your dentist detects gum disease early, they may recommend professional cleaning to address the issue. The procedure involves the removal of plaque and tartar build-up, which can prevent further infection and promote healthy gum reattachment to the teeth.
To perform the cleaning, the dentist will use a scaler to scrape off plaque and tartar from your teeth. They will then use a specialized tool called a prophy cup to polish your teeth, resulting in a smoother tooth surface more resistant to plaque and tartar build-up.
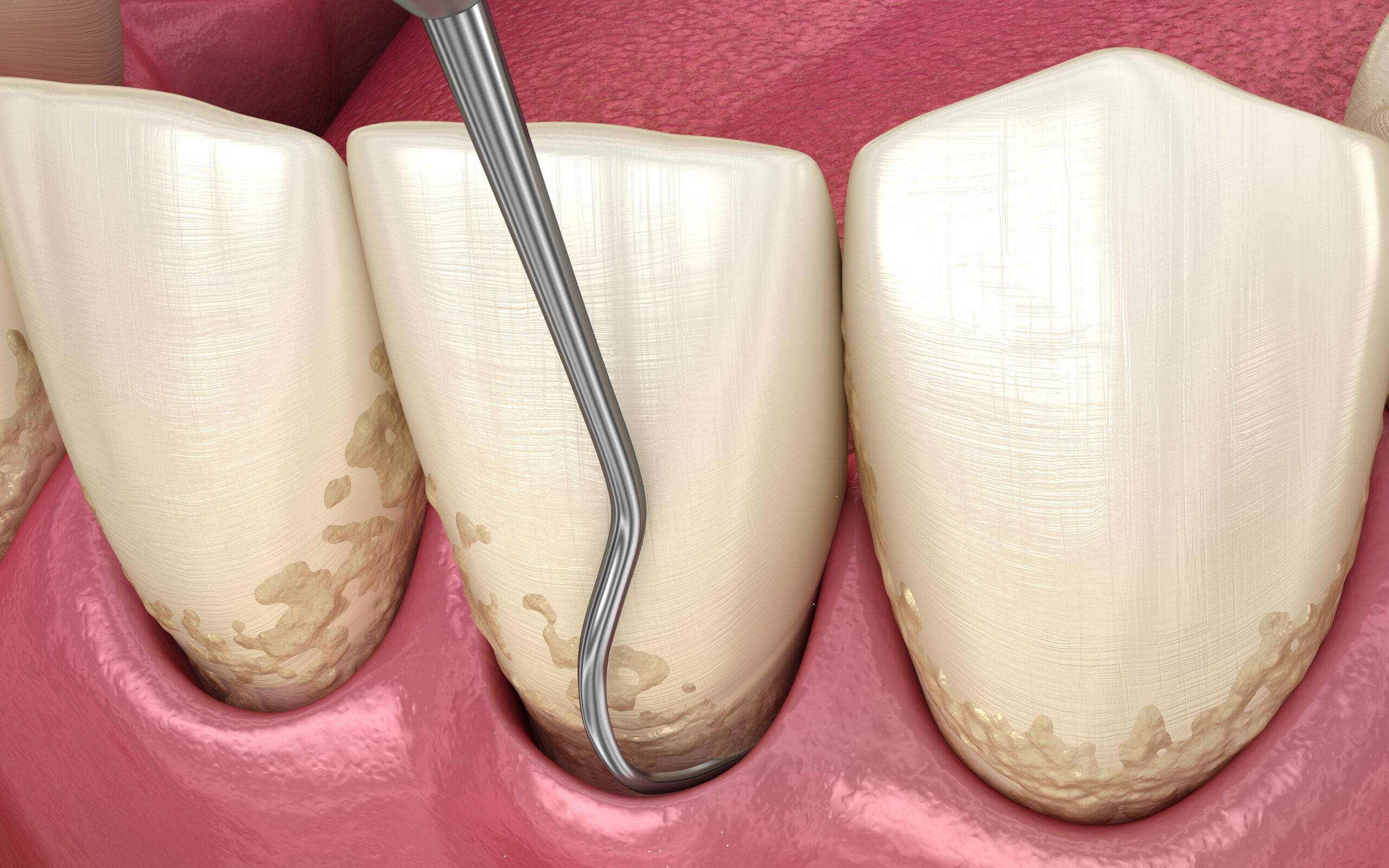
Scaling and Root Planing
Periodontitis can be effectively treated with a non-surgical procedure called scaling and root planing. This procedure involves removing plaque and tartar build-up above and below the gum line.
To ensure your comfort, your dentist will administer local anesthesia to numb the gums surrounding the affected teeth. Following this, a dental scaler will be used to carefully remove tartar from the surface of your teeth and areas below the gumline. Sometimes, an ultrasonic scaler may also be used to loosen tartar deposits.
After removing the tartar, your dentist uses a dental curette to smooth the roots of your teeth. This process, known as root planing, promotes the healthy reattachment of gums and makes it more difficult for bacteria to attach to the tooth.
Antibiotic Therapy
Your dentist may recommend antibiotic therapy if your gum disease has progressed to the point where the infection has spread into the soft tissue and supporting structures of the teeth,
To determine the specific bacteria causing the infection, your dentist will carry out a saliva test and, based on the results, prescribe an effective antibiotic against the infection. Commonly prescribed antibiotics against gum disease include tetracycline hydrochloride, doxycycline, and minocycline.
The antibiotics may be administered in various ways, including injections directly into the affected area, creams applied to the infection site, and capsules to be taken orally. The method of administration depends on the location and severity of the infection.
Surgical Gum Disease Treatment Options
Flap Surgery
Flap surgery is a procedure that involves the removal of bacteria and tartar deposits from the pockets formed between the teeth and gums. If non-surgical procedures like scaling and root planing prove ineffective, your dentist may recommend flap surgery.
The procedure begins with your dentist numbing the surgical site using local anesthesia. A small incision is then made in the gum tissue to create a flap, which allows the dentist to reveal the tooth’s root and supporting bone structure.
Using specialized instruments, the dentist removes the tartar build-up from the exposed root and supporting bone structures. Once the tartar is removed, the flap is repositioned to reduce the depth of the gum pockets and sutured back into place.
Bone and Tissue Grafts
Advanced gum disease can lead to the destruction of bone and soft tissue that support your teeth. Your dentist may recommend bone and tissue grafts to restore these structures. Graft material can come from various sources, such as healthy parts of your own body, cadaver tissue and bones, and synthetic materials.
Your dentist will administer local anesthesia to numb the surgical site to minimize discomfort. However, general anesthesia may be necessary for extensive grafting procedures.
Once you are comfortable, the dentist will make an incision in the gums to expose the graft site. Next, the graft material is placed on the prepared site.
After the graft material is in place, the gum tissue is sutured back over the graft site to stabilize the graft and promote healing.
Guided Tissue Regeneration
Guided tissue regeneration is a surgical procedure used to treat advanced gum disease and promote the growth of bone and tissue that the infection may have damaged. It involves placing a mesh-like barrier between the gum tissue and bone to prevent the gum tissue from growing into bone defects.
Your dentist will administer local anesthesia to numb the surgical site to alleviate discomfort during the procedure. In some cases, general anesthesia may be recommended depending on the procedure’s nature.
After ensuring you’re comfortable, the dentist will make an incision to expose the affected area. Following this, they will carefully remove diseased tissue from the affected area and place a mesh-like barrier over it.
This barrier promotes healthy bone and gum tissue regeneration by preventing the gum tissue from growing into bone defects. Once the barrier is in place, the dentist will suture the gum tissue back over the surgical site to hold the barrier in place and promote healing.
Post-Treatment Care
After your treatment, your dentist may recommend the following instructions to promote healing and prevent recurring gum infections.
- Avoid smoking: Cigarette smoke contains substances that can wreak havoc on your oral structures, delay healing and increase your risk of developing gum disease
- Use antibacterial mouthwash: Rinsing with mouthwash can help kill bacteria in hard-to-reach areas of the mouth. Your dentist may recommend a specific mouthwash that’s gentle on your gums
- Practice good oral hygiene: Be sure to maintain good oral hygiene after treatment. Brush at least twice daily using a soft-bristled brush and floss gently to remove plaque from between your teeth
- Attend regular dental check-ups: Regular appointments will allow your dentist to examine your progress and address any possible complications
- Watch your diet: Avoid sugary and acidic foods that can hinder healing and contribute to tooth decay. Go for foods rich in vitamins and minerals as they promote healing and boost your immunity

Note, the post-treatment care tips mentioned above can serve as effective measures for preventing gum disease from occurring in the first place.
Gum disease is a severe condition that can significantly impact your quality of life, but the good news is that effective treatment options are available. Professional teeth cleaning, scaling and root planing, flap surgery, and bone grafts are all effective ways to address gum disease and reverse the damage caused by infection.
If you are concerned about gum disease, it is important to consult your dentist. Early detection is crucial for saving your teeth and preventing the disease from progressing to a more severe stage.
Visit Us Today!
We look forward to meeting you. Call (910) 469-1049 or request an appointment online to set up your first visit. We’ll be in touch soon.
O2 Dental Group of Southern Pines
(910) 469-1049
Monday:
Tuesday:
Wednesday:
Thursday:
Friday:
Saturday:
Sunday:
8:00am – 6:00pm
8:00am – 6:00pm
8:00am – 6:00pm
8:00am – 4:00pm
CLOSED
CLOSED
CLOSED

