Root Canal Treatment Durham, NC
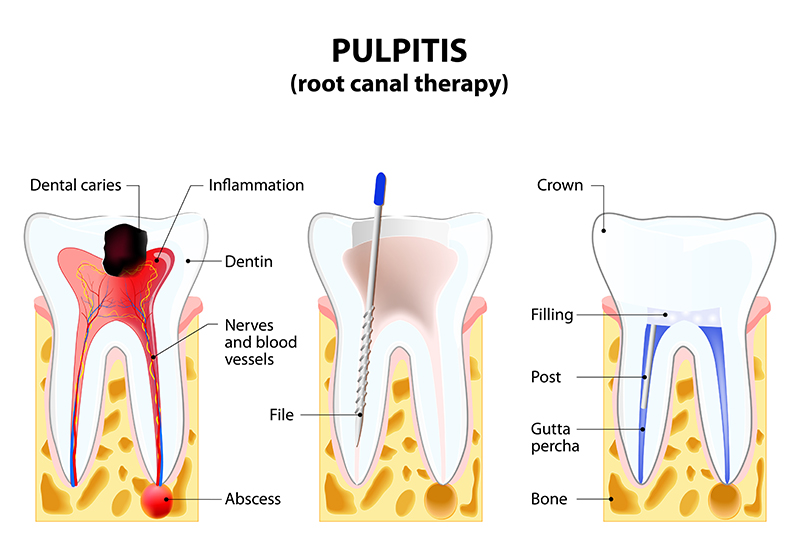
Root canal treatment (endodontic treatment) is a restorative dental procedure to repair a damaged tooth. When the tooth’s pulp is exposed due to enamel damage or cavities, it can become inflamed, causing severe pain and discomfort.
Root canal therapy involves removing the infected pulp, cleaning the pulp chamber, and filling it with a biocompatible material. A dental crown then seals the tooth, restoring its functionality and strength.
When Is a Root Canal Needed?
The dental pulp in the tooth’s center is a living tissue of nerves and blood vessels. The pulp nourishes the tooth and allows it to sense pressure and temperature changes.
Tooth trauma and deep cavities can compromise the pulp, causing inflammation or infection. Pulp damage can cause severe pain and serious health complications. In most cases, root canal therapy may be necessary to remove the damaged pulp and restore the tooth.
What Can You Expect During a Dental Filling Procedure?
The dental pulp in the tooth’s center is a living tissue of nerves and blood vessels. The pulp nourishes the tooth and allows it to sense pressure and temperature changes.
Tooth trauma and deep cavities can compromise the pulp, causing inflammation or infection. Pulp damage can cause severe pain and serious health complications. In most cases, root canal therapy may be necessary to remove the damaged pulp and restore the tooth.
Your dentist might recommend endodontic treatment if your tooth has the following symptoms:
- Severe tooth pain: Intense tooth pain, especially when biting and chewing, is a common sign of pulp damage. Temperature changes might also trigger persistent tooth pain.
- Abscess: An abscess is a puss-filled pocket that forms on the gum in cases of severe pulp damage. Abscess forms when the bacteria infecting the pulp spreads to the gum tissue.
- Tooth discoloration: Pulp damage and infection can interrupt blood supply to the tooth. The lack of adequate nourishment will result in the tooth turning black.
- Bad breath: A bacterial infection of the pulp might cause bad breath and a foul taste in the mouth if left untreated.
- Inflamed gums: An infected pulp can aggravate the gums surrounding the tooth, causing inflammation and tenderness.
Root Canal Procedure
Root canal therapy is a straightforward procedure that can take a few hours, depending on your situation. The process involves the following steps:
Evaluation
First, your dentist takes dental X-rays of the affected tooth. The resulting image helps them examine the tooth and decide the best approach for the root canal procedure.
Anesthesia
Next, the dentist administers local anesthesia to numb the affected tooth and surrounding gums.
You may be given oral sedatives to help you relax if you have dental anxiety. Once you’re comfortable, the dentist places a dental dam in your mouth. The rubber-like sheet isolates the tooth, keeping it clean and saliva-free.
Access Opening
The dentist makes an opening in the crown of the affected tooth using a dental drill or a dental laser. He will then use specialized dental instruments to access the pulp chamber through this opening.
Pulp Removal
This is a critical step of the root canal procedure. The dentist carefully cleans the pulp chamber using dental files of different sizes and shapes. They start from the pulp chamber and carefully progress down the root canals.
Next, the dentist shapes the root canals using specialized rotary files. During this process, they smooth the walls of the pulp chamber and canals to create a uniform shape for the filling material.
The dentist flushes the pulp chamber using irrigation solutions, removing bacteria and debris. As a precaution, the dentist may use a microscope to examine the pulp chamber for any residual inflamed tissue.
Filling the Canals
Once the dentist ensures the root canal is clean and dry, they fill it with a biocompatible rubber-like material called gutta-percha. The specialized material is inserted in the canals in increments. The dentist uses a specialized heating instrument to soften the filling and ensure it flows uniformly into the root canal.
The gutta-percha is then compacted to form an airtight seal in the pulp chamber and canals. Finally, the dentist covers the access opening with a temporary filling. The temporary filling protects the canals from food and saliva damage until a permanent crown can be placed.
Final Restoration
Depending on the tooth’s location, function, and structural integrity, your dentist may recommend a dental crown or permanent fillings. A dental crown is the best option if there isn’t enough healthy tooth structure remaining and if the tooth undergoes constant stress during normal function.
The crown has to be custom-made to fit your tooth. Since fabricating a permanent crown takes a few days, the dentist will place a temporary crown to protect the tooth.
Your dentist will set up an appointment for the final restoration once the permanent crown is ready. The procedure takes a few minutes. The dentist removes the temporary crown and cleans the tooth. He then will place the permanent crown and cement it in place using dental adhesive.
Postoperative Care For Root Canal Treatment
Proper aftercare for root canal treatment ensures quick recovery and prevents complications. Your dentist will advise that you follow specific postoperative care instructions.
They include:
- Take medication as prescribed: Depending on your situation, the dentist may prescribe antibiotics and pain medication. Taking the medication as prescribed reduces discomfort and the risk of infection.
- Practice good oral hygiene: After the procedure, you should maintain good oral hygiene. However, avoid damaging the treated tooth through aggressive brushing and flossing.
- Watch your diet: Avoid hard , and crunchy foods for a few days after the procedure or until you have received your permanent restoration. Such foods might damage the temporary crown and hinder your recovery.
- Avoid smoking: Cigarette smoke contains harmful chemicals like hydrogen cyanide that drastically slow healing. It would be best to avoid smoking for a few weeks after the procedure. This is especially important if you have undergone endodontic surgery such as an apicoectomy.
- Attend follow-up appointments: Be sure to attend follow-up appointments. Regular checkups allow your dentist to check for complications and determine whether the tooth is healing.
- Use a cold compress: A cold compress on the affected area will help reduce swelling and discomfort. However, you should contact your dentist immediately in case of persistent pain, swelling, and discomfort.
While the healing time for a root canal varies, following postoperative care instruction ensures a speedy recovery. You’ll experience slight discomfort for a few days after the procedure as the tooth, and the surrounding tissues recover.
In general, the treated tooth will regain full functionality after a week. However, the full healing process might take several weeks in some cases.

Possible Dental Complications and Risks of Root Canal Treatment
While root canal therapy is a straightforward procedure, there are various risks associated with the treatment.
These include:
Damage to the Surrounding Teeth and Tissue
The dentist may need to remove some tissue to access the affected tooth properly. Rarely, this could result in damage to the surrounding teeth.
Infection
There is a slight risk of infection after the root canal procedure. Infection can take root if bacteria from the mouth infect the treated tooth. Also, improper tooth cleaning during the procedure might result in an infection.
Allergic Reactions
In rare cases, you might develop an allergic reaction to the filling material. However, this is unlikely since gutta-percha is a biocompatible material. If you develop an allergy, your dentist will replace the gutta-percha with alternatives such as Resilon.
Nerve Damage
The root canal procedure may damage the nerves surrounding the affected tooth. Common signs of nerve damage include tingling in the surrounding area and numbness. However, this rarely happens when performed by skilled clinicians.
Delayed Healing
Sometimes, the treated tooth might not heal properly, causing pain, discomfort, and possible infection. Delayed healing may be due to improper canal cleaning during the procedure and poor postoperative care. In some cases, a tooth may not respond to endodontic treatment due to undetected root fracture or advanced damage or decay or a number of other reasons.
Fracture of the Tooth
The treated tooth might become structurally weak after the procedure. However, placing a dental crown reduces the risk of the tooth developing a fracture over time.
It’s important to note that the risks associated with root canal treatment rarely occur if you follow the postoperative care instructions given by your dentist. However, you should immediately seek medical attention if you experience any of the following symptoms after your procedure.
- Fever, nausea, and vomiting
- Numbness and tingling in the lips, tongue, and area surrounding the treated tooth
- Bad breath and a foul taste in your mouth
- Cracks developing on the treated tooth
- Inflammation of the gums surrounding the treated tooth
- Discharge or pus coming from the treated tooth
Your endodontist may prescribe medication or recommend retreatment to address the issues and avoid further complications.
Root Canal Alternatives
There are situations where root canal treatment is not possible or necessary.
Examples include:
- Minor decay: Cases of minor decay can be treated by non-invasive procedures such as crown placement and dental fillings
- Non-restorable tooth: Root canal isn’t necessary if the tooth is too badly damaged or broken down. Your dentist might recommend extraction if there are no restorative options to save your tooth..
- Medical complications: Certain medical conditions, such as heart disease, make undergoing a root canal too risky. Your dentist will recommend alternative treatment in such cases.
Though root canal therapy is a safe and effective treatment for pulp infection, your dentist may recommend alternatives such as:
Pulpotomy
This procedure involves removing only the infected and inflamed portions of the pulp. A protective filling is then used to seal the pulp chamber and protect the remaining healthy pulp. However, this procedure is only effective for treating minor pulp infections. This is considered a temporary solution before the root canal can be completed.
Dental Restoration
Your dentist may recommend non-invasive dental restoration procedures in cases of minimal tooth damage. These include structures such as fillings and crowns to strengthen the damaged tooth.
Tooth Extraction
Tooth extraction may be the only solution if root canal therapy and other dental procedures can’t save the tooth. It’s important to note that tooth extraction is usually a last resort.
Root canal treatment can seem daunting at first. However, dental technology and medical advances have made it a quick and painless procedure. Moreover, root canal therapy can restore your tooth’s function and prevent tooth loss through extraction. For the best results, consult a skilled dentist or endodontist on root canal therapy and other dental restorative procedures.
Schedule Today!
We look forward to meeting you. Call (919) 646-3849 or request an appointment online to set up your first visit. We’ll be in touch soon.
O2 Dental Group of Durham
(919) 646-3849
Monday:
Tuesday:
Wednesday:
Thursday:
Friday:
Saturday:
Sunday:
9:00am – 5:00pm
9:00am – 5:00pm
9:00am – 5:00pm
9:00am – 5:00pm
8:00am – 2:00pm (every other Friday)
CLOSED
CLOSED

