Disclaimer: This article is for informational purposes only. O2 Dental Group does not offer transosteal implants. We only offer the endosteal implant procedure.
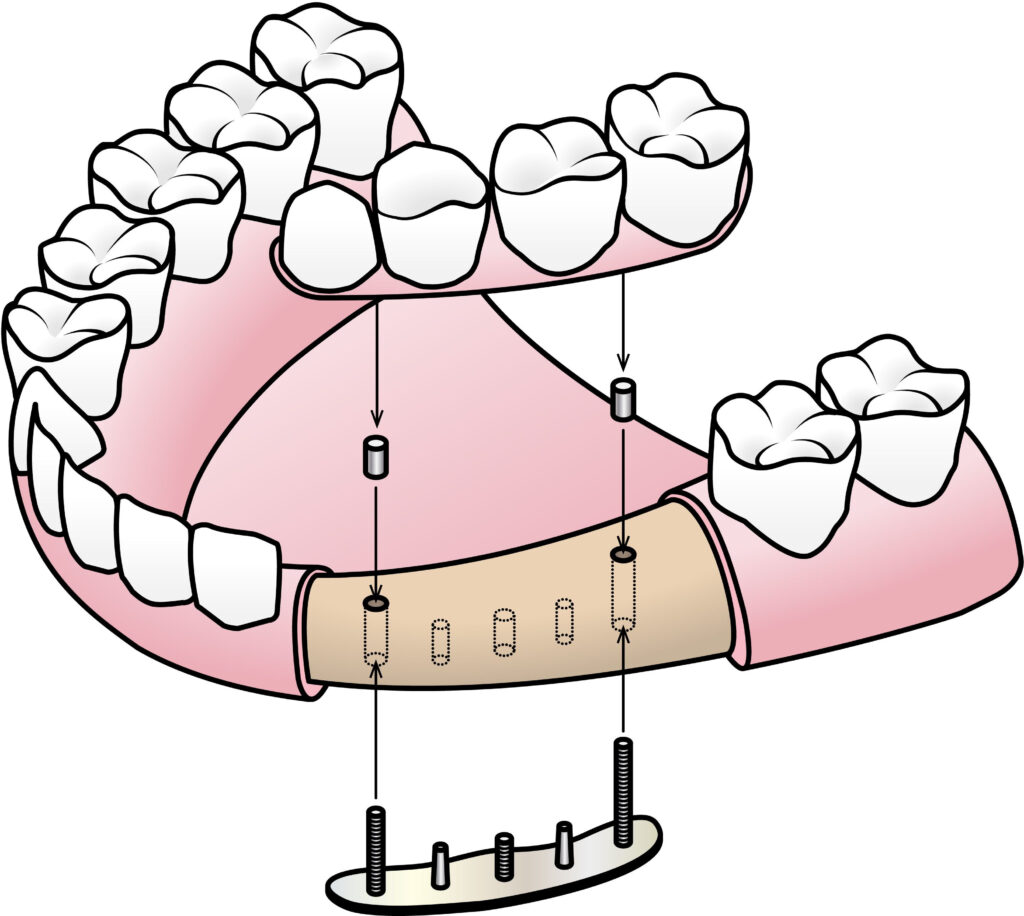
Transosteal implants are used in dental restoration procedures when traditional implants are not feasible. Unlike endosteal implants, transosteal implants are inserted through the jawbone and secured to a horizontal metal plate bolted to the underside of the lower jaw.
Transosteal implants are recommended for patients with inadequate bone density to support traditional implants due to severe bone resorption. Since transosteal implants require a more complex and extensive surgical procedure than traditional implants, reliable information is crucial to making an informed decision.
This article covers the benefits, risks, and suitability of transosteal implants. It also provides accurate information on the placement process, implant cost, success rates, and potential risks associated with transosteal implants.
Find out why transosteal implants are an effective dental restoration solution and whether they are a viable option for your oral health needs.
What Are Transosteal Implants
Transosteal implants are a type of dental implant used to replace missing teeth for patients with insufficient jawbone density. Transosteal implants consist of posts inserted through the jawbone and attached to a metal plate secured beneath the mandible.
Benefits of Transosteal Implants
Transosteal implants have the following benefits for patients with missing teeth:
- Stability: Transosteal implants are highly stable due to their unique design. The metal plate attached to the jawbone provides dental prosthesis attached to the transosteal implants with a stable and secure foundation
- Multiple teeth support: Transosteal implants can support multiple teeth or even a full arch of teeth, making them an ideal restoration solution for patients who require extensive tooth replacement
- Durability: Transosteal implants are made of titanium, which is known for its strength and biocompatibility. As a result, transosteal implants can last for decades with the proper care and maintenance
- Shorter treatment time: Transosteal implants require fewer surgeries and additional procedures than alternative dental restoration treatments. Moreover, dental prostheses can be attached immediately after implant placement in some situations. As such, transosteal implants have a shorter treatment time.
- Versatility: Transosteal implants are a versatile treatment option since they can be used in various dental scenarios. For instance, the implants can be anchored in the stable areas of the jawbone, eliminating the need for extensive bone grafting. They can also support various types of dental restorations, including implant-supported dentures, partials, single crowns, and bridges
Transosteal Implants vs Regular Implants
Differences Between Transosteal Implants and Traditional Implant Options
Though transosteal, endosteal, and subperiosteal implants are effective dental restoration options, they have notable differences. For example, transosteal implants replace missing teeth in the lower jawbone. On the other hand, endosteal implants are more versatile. They can be used for the lower and upper jawbone.
Regarding surgical procedures, placing transosteal implants is more complex and extensive than traditional implants. The surgical procedure for transosteal implants involves inserting titanium posts through the jawbone and attaching them to a metal plate beneath the mandible.
In contrast, endosteal implants are placed directly into the jawbone without passing through it, while subperiosteal implants are placed beneath the gum tissue but on top of the jawbone.
Transosteal implants can be used in cases of severe bone loss since the implants can bypass the inadequate bone regions and provide stability by anchoring in the denser jawbone areas. Subperiosteal implants are also an effective alternative for patients with inadequate bone density. Since the metal framework is placed on top of the jawbone, subperiosteal implants can be used as a replacement option for patients with severe bone resorption.
A significant disadvantage of transosteal implants is their recovery period. Since the complex surgical procedure involves penetrating the jawbone in multiple areas, the recovery period of transosteal implants may be longer and involve more discomfort than traditional implants.
Transosteal Implant Placement
Evaluation
Your dentist will schedule a dental examination to evaluate your viability for transosteal implants. They will conduct tests, including X-rays, CT scans, and oral examinations, to assess your bone density and overall oral health. The dentist will also evaluate your medical history to determine whether any underlying issues might complicate the procedure. Once satisfied with the results, your dentist will create a unique treatment plan suited to your oral health needs.
Anesthesia Administration
Your dentist will administer anesthesia to ensure your comfort during the procedure. Though local anesthesia can be used to numb the surgical site, your dentist may recommend general anesthesia depending on the complexity of the procedure or if you have a severe case of dental anxiety.
Bone Preparation
Once the anesthesia has taken effect, your dentist will make a small incision below the chin to expose the lower jawbone and create the necessary space for the metal plate. They will then drill pilot holes through the jawbone. These pilot holes create pathways for the transosteal pins to the metal plate.
Implant and Metal Plate Placement
Next, your dentist will position a metal plate made of titanium beneath the jawbone. The transosteal pins are inserted through the pilot holes and secured to the metal plate using special nuts. The metal plate can be custom-made to accommodate multiple attachment points. It also provides a stable foundation for the transosteal pins ensuring they are firmly anchored.
Your dentist will then close the incision beneath the chin and carefully suture the gum tissue around the transosteal posts to promote proper healing. They will cover the implant posts with protective caps to prevent infection while the implants fuse with the jawbone through osseointegration.
Artificial Teeth Attachment
Once the gum tissue has healed and the implants have fused with the jawbone, your dentist will remove the protective caps and attach the replacement teeth or dental prosthesis to the transosteal posts. The prosthetic teeth are designed to match the shape and color of your natural teeth, providing a functional and aesthetic replacement for missing teeth.
Transosteal Implant Cost
The following factors can affect the cost of transosteal implants:
- Complexity of the surgical procedure: Placing transosteal implants involves a complex multistep process that may affect the cost of the procedure. Moreover, the overall cost may increase if additional procedures, such as bone augmentation, are required
- Number of implants: Multiple replacement teeth can be attached to transosteal implants. Since most dental practices charge per implant, each additional implant will add to the overall cost.
- Customization: Transosteal implants must be customized to fit the width and height of a patient’s jawbone. The customization process may increase the overall cost as it involves expertise and additional labor.
- Geographic location: The geographic location of your dental care provider can significantly affect the cost of transosteal implant placement. For example, overhead costs and competition between dental practitioners can influence pricing.
- Implant material: Premium-quality transosteal implants made of high-quality titanium or ceramic may be more expensive than generic implants.
- Diagnostic tests: Special diagnostic and imaging tests, such as CT scans, digital impressions, and X-rays, may be carried out during the initial evaluation. These tests can increase the overall cost of the procedure.
It’s important to note that though transosteal implants may cost more than alternative dental restoration options, they have several long-term benefits that justify the investment. These include:
- Improved chewing function
- Jawbone preservation
- Enhanced aesthetics
- Improved speech function
- Longevity
Safety and Success Rate of Transosteal Implants
Potential Risks and Complications Associated With Transosteal Implants
Infection
As with all implant procedures, transosteal implant placement carries a risk of infection. Harmful bacteria might accumulate around the implant site leading to infection, especially if the patient doesn’t follow post-operative instructions.
Surgical Complications
Transosteal implant placement is a complex surgical procedure. Various complications may occur, including allergic reactions to anesthesia, frequent bleeding, and damage to surrounding teeth. Moreover, long-term complications such as nerve damage and implant rejection are also a possibility.
Implant Failure
Any dental implant carries a risk of failure. Transosteal implants can fail for various reasons, including poor integration with the bone, mechanical problems with the implant components, and inadequate stability. Since failed implants require removal, additional surgical procedures can lead to further complications.
Soft Tissue Complications
Since transosteal implants pass through soft tissues, the patient may develop complications such as ulceration, tissue irritation, and gum recession. Adjustments to the implant components and tissue grafting may be necessary to address these complications.
Success Rate and Reliability of Transosteal Implants.
Though there are various risks associated with transosteal implants, studies have shown that they are a reliable dental restoration solution with a high success rate. For example, a study published in the Journal of Oral Science and Rehabilitation found that transosteal implants have a success rate of 74% and a survival rate of 100% after definitive prosthetic rehabilitation.
The study also found that age, sex, habits, and systemic diseases do not significantly influence the success rate of transosteal implants, making them a versatile dental restoration option.
Factors that Contribute to the Success of Transosteal Implants
The success of transosteal implants can be influenced by several factors, including the following:
- Surgical Technique: Transosteal implant placement involves an extensive and complicated surgical procedure. Proper implant placement and correct angulation are crucial to achieving implant stability. As a result, choosing a skilled surgeon who specializes in transosteal implants increases the chances of success
- Bone quality and quantity: Though transosteal implants can be used in cases of severe bone resorption, a healthy and solid jawbone ensures implant stability. Moreover, transosteal implants require adequate jawbone width and height to ensure a proper fit.
- Patient lifestyle: Certain lifestyle choices can affect the success rate of transosteal implants. For example, smoking impedes healing and increases the risk of implant failure. As a result, smokers are advised to quit smoking for at least six months before implant placement.
- Post-surgical care: Following the post-surgical care instructions as advised by your dentist is crucial for the success of transosteal implants. These include taking prescribed medication, following a soft diet, and observing proper oral hygiene habits.
- Follow-up care: Attending follow-up appointments allows your dentist to monitor the implant and address potential complications. Your dentist may also make necessary adjustments to the implant framework to increase its lifespan
Transosteal Implant Recovery and Timeline
Transosteal Implant Recovery Process
Post-operative Care
It’s normal to experience pain, discomfort, and bleeding after transosteal implant surgery. Your dentist will prescribe pain medication to address the pain and relieve discomfort. They will also place a protective gauze over the surgical site to control the bleeding. At-home remedies such as applying ice packs and warm compresses to the affected area can help reduce swelling and promote healing.
Diet
Watching your diet during the initial days following the surgery promotes healing and reduces the risk of complications. Avoid sticky, crunchy, and spicy foods that may irritate the implant site. Instead, observe a soft diet that includes yogurt, soups, mashed potatoes, applesauce, and smoothies.
Oral Hygiene
Maintaining good oral hygiene reduces the risk of infection and implant failure. Your dentist will provide specific instructions on how to clean your teeth. This may include rinsing your mouth with a prescribed mouthwash and gently cleaning your teeth using a soft-bristled toothbrush.
Follow-up Appointments
Your dentist will schedule follow-up appointments to monitor your recovery progress. These appointments are essential to the healing process. For example, your dentist will address any concerns regarding the implant. They will also examine the implant site and address any potential issues before they worsen.
Healing and Integration Timeline for Transosteal Implants
Though the healing and integration timeline for transosteal implants can vary depending on various factors, here’s a general outline of the process:
- Initial healing: The healing process begins after the surgery and lasts 2 to 3 weeks. It’s normal to experience swelling, discomfort, and minor bleeding during this period. Following post-care operative care instructions, such as taking prescribed pain medication and sticking to a soft diet, can help manage these symptoms.
- Osseointegration: The jawbone gradually fuses with the implant’s surface during osseointegration. This process takes approximately 3 to 6 months. Maintaining good oral hygiene and attending regular checkups promotes proper healing and reduces the risk of complications during this phase.
- Prosthetic attachment: Dental prostheses such as bridges or dentures can be attached to the transosteal implants once osseointegration is complete. Your dentist may place connectors on the implant to serve as attachment points for the replacement teeth
- Final adjustments: Your dentist will schedule regular checkups to monitor the implant and make any necessary adjustments to enhance its longevity and functionality
Potential Disadvantages of Transosteal Implants
While transosteal implants offer various advantages, you should consider their potential drawbacks and disadvantages. They include the following:
- Surgical complexity: Transosteal implants require a more complex surgical procedure than other options. Unlike endosteal and subperiosteal implants, transosteal implants are inserted through the jawbone. The complexity of this procedure may limit the availability of transosteal implants and increase the overall cost
- Invasiveness: Transosteal implant surgery is typically more invasive than endosteal and subperiosteal placement procedures. The invasive procedure may lead to a longer healing time and increase the risk of complications
- Cost: Since transosteal implants need to be customized according to the width and height of the jawbone, they may cost more than regular implants. Additionally, the complex surgical procedure may increase the overall cost
- Maintenance: The design of transosteal implants, which involves protruding posts running through the jawbone, can make cleaning and maintenance challenging. Plaque might accumulate around the metal posts, increasing the risk of implant failure and gum disease
- Bone quality requirements: Though transosteal implants are often recommended for patients with bone loss in the jaw, individuals with poor bone quality and quantity may not be suitable candidates for the implants
Alternative Dental Restoration Options for Transosteal Implants
The following dental restoration options can provide alternatives for patients who aren’t suitable candidates for transosteal implants:
- Subperiosteal implants: Subperiosteal implants are placed on top of the jawbone but beneath the gum line, making them a great alternative for patients with insufficient bone density to support transosteal implants
- Dental implant-supported dentures: These dentures are attached to the jawbone using a few strategically placed implants. The implants can support multiple replacement teeth and can be used as an alternative for patients with insufficient bone height and density
- Dental bridges: A dental bridge consists of artificial teeth, called pontics, anchored to adjacent healthy teeth on either side of the gap. Dental bridges are an effective restoration solution that can be used to replace one or more missing teeth
- Complete dentures: Complete dentures are affordable dental prostheses that can replace multiple missing teeth in the upper or lower jaw. They are made of artificial teeth supported by a metal framework that attaches to the remaining healthy teeth
Transosteal implants offer various advantages for patients seeking a reliable and durable dental restoration solution. By anchoring directly into the jawbone, transosteal implants provide stability and support for replacement teeth, especially in cases where traditional implants aren’t feasible.
Moreover, transosteal implants distribute forces evenly across the jawbone, increasing the durability of the dental prosthesis and enhancing chewing functionality. However, factors such as bone density, medical history, and oral health can affect the viability of these implants.
Therefore, you should consult your dentist to determine whether transosteal implants are a viable treatment option. They will help you make an informed decision by evaluating your oral health and considering your specific needs and preferences.